Rheumatoid Arthritis (RA)
Understanding, Managing, and Living Well
What Is Rheumatoid Arthritis (RA)?
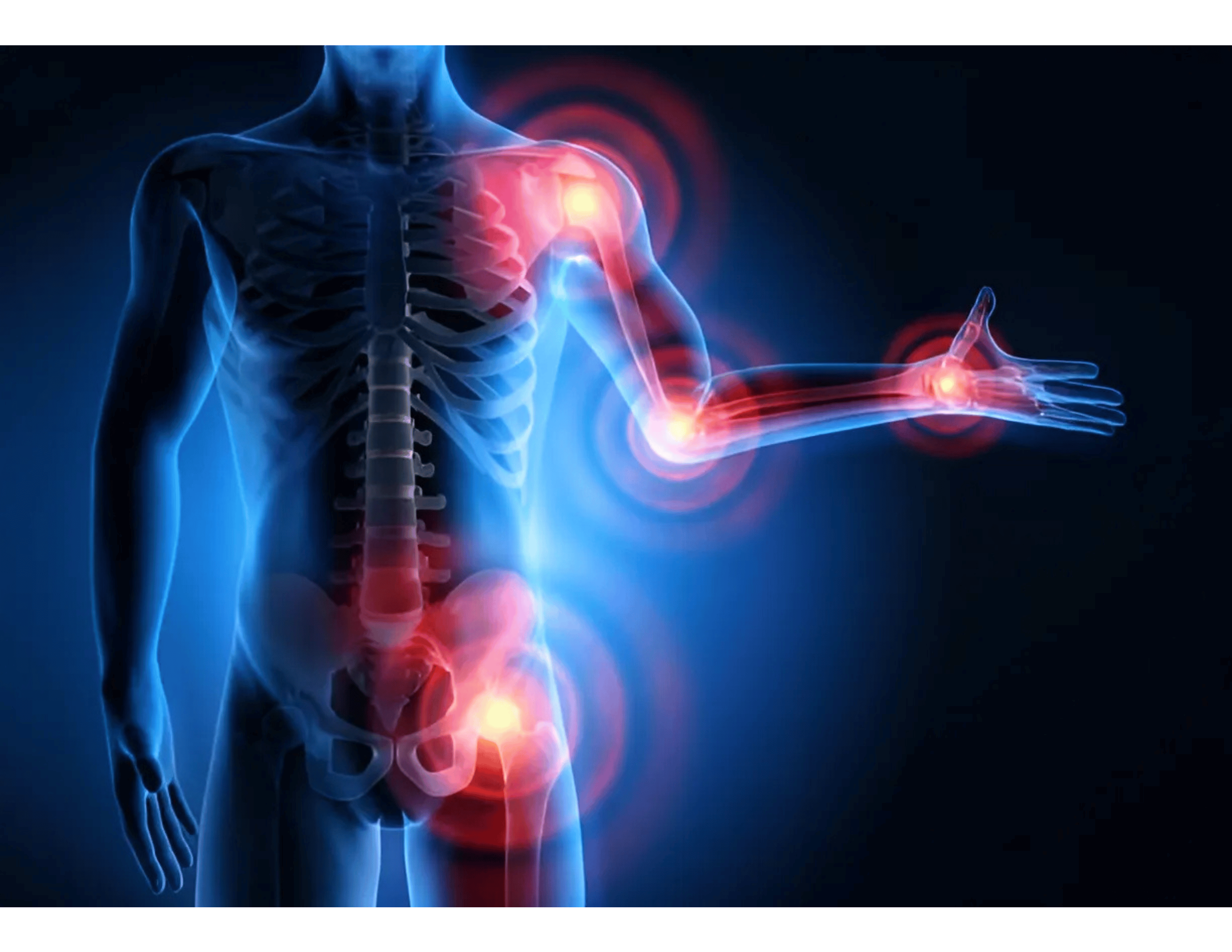
Rheumatoid arthritis (RA) is an autoimmune disease, which means your immune system mistakenly attacks your own body. Specifically, rheumatoid arthritis targets the joints, leading to inflammation, pain, and even joint damage over time. Unlike osteoarthritis, which is typically due to wear and tear, rheumatoid arthritis is a chronic inflammatory condition that can affect anyone, although it is more common in certain groups. It is considered a lifelong disease, but with the right treatments and support, you can manage it effectively.
When Does Rheumatoid Arthritis Begin?
Rheumatoid arthritis (RA) can start at any age but most often appears between ages 30 and 60. Juvenile Rheumatoid Arthritis (JRA), can affect children under 16. While symptoms can develop quickly, rheumatoid arthritis generally progresses over time, with early symptoms often mistaken for other issues. If you notice joint pain, stiffness, or swelling that persists, it may be worth talking to your doctor.
Is Rheumatoid Arthritis Hereditary?
Rheumatoid arthritis has a genetic component, meaning if you have family members with RA, you might have a higher risk of developing it. So, yes, genetics can influence your likelihood of developing rheumatoid arthritis. However, rheumatoid arthritis isn’t directly passed down from parent to child. Instead, certain genetic markers make you more susceptible, especially if combined with other risk factors like smoking or exposure to environmental triggers.
Studies have identified several genes associated with rheumatoid arthritis, particularly in people of European descent. However, simply carrying these genes doesn’t mean you’ll get RA; it just increases your risk.
Does Rheumatoid Arthritis Affect Men and Women Equally?
Rheumatoid arthritis affects women about two to three times more often than men. The reasons for this disparity aren’t fully understood, but it may be linked to hormonal factors. Many women report that symptoms worsen during certain hormonal changes, such as pregnancy or menopause. Men who develop rheumatoid arthritis may experience more severe symptoms, but they represent a smaller percentage of those diagnosed.
What Triggers Rheumatoid Arthritis?
While the exact cause of rheumatoid arthritis remains unknown, experts believe it results from a combination of genetic and environmental factors. Here are some potential triggers:
Genetics: Certain genes are associated with a higher risk of developing Rheumatoid Arthritis.
Infections: Viral infections may prompt immune responses that lead to RA.
Hormones: Changes in estrogen levels may play a role, as women are more likely to develop rheumatoid arthritis.
Environmental Factors: Smoking, exposure to pollution, and even some viruses and bacteria may increase the risk.
Stress and Trauma: Physical or emotional stress may also trigger symptoms in those predisposed to rheumatoid arthritis.
Diet and Gut Health: Some research suggests that gut bacteria play a role in autoimmune diseases, and dietary factors may influence gut health and inflammation.
Fact: Quitting smoking is one of the most effective lifestyle changes for lowering your RA risk, especially if you have a family history of the condition.
Symptoms of Rheumatoid Arthritis
RA can vary significantly from person to person, but common symptoms include:
- Joint pain, swelling, and stiffness: Particularly in small joints of your hands and feet, along with warmth and redness.
- Stiffness: Especially noticeable in the morning or after periods of inactivity.
- Fatigue and Fever: General feelings of tiredness, sometimes accompanied by a low-grade fever.
- Symmetry: RA often affects joints symmetrically, meaning both sides of the body experience symptoms.
- Joint deformities: Rheumatoid arthritis can develop into structural changes to the joints and ligaments in the hands, and can severly worsen if untreated.

Can Cold Weather and Seasonal Changes Affect The Severity of Rheumatoid Arthritis?
Yes, cold weather and seasonal changes can affect the severity of Rheumatoid Arthritis (RA) for many individuals. While the connection between weather and rheumatoid arthritis symptoms is not fully understood, many people with RA report experiencing increased joint pain and stiffness during colder months or when the weather changes. Here are a few reasons why cold weather may influence RA symptoms:
Temperature and Joint Stiffness: Cold temperatures can cause muscles to contract, which may increase joint stiffness and make movement more painful for those with RA.
Barometric Pressure: Changes in barometric pressure, which often occur before weather shifts, can put additional pressure on the joints. This can lead to increased discomfort in people with arthritis.
Reduced Physical Activity: Cold weather may discourage people from staying active. Physical activity is essential for maintaining joint flexibility and managing RA symptoms. Less movement can lead to increased stiffness and pain.
Inflammation Response: Some studies suggest that the cold may increase inflammatory responses, which could potentially worsen RA symptoms.
Seasonal Mood Changes: During the winter months, people are more prone to Seasonal Affective Disorder (SAD) or depression due to reduced sunlight exposure. Depression can exacerbate pain perception, leading to a perceived increase in RA severity.
However, it’s important to note that the impact of cold weather on RA can vary from person to person. While some may feel worse in cold or damp weather, others may not experience much change at all or may even feel more comfortable during these times. To manage symptoms during colder seasons, people with RA can try the following:
- Dress warmly in layers to keep joints comfortable.
- Use heating pads or warm baths to relieve stiffness.
- Stay physically active, even indoors, with exercises like stretching, yoga, or swimming in a heated pool.
- Maintain a healthy, anti-inflammatory diet to help control overall inflammation.
If weather changes significantly affect RA severity, consulting with a healthcare provider for personalized strategies may also be helpful.
Fun Myths and Trivia About Rheumatoid Arthritis
Rheumatoid arthritis is one of the most common misunderstood medical conditions. With some facts and lots of misconceptions surrounding it, let’s clear up a few:
Myth
Fact
Trivia
Rheumatoid Arthritis is just like “normal” arthritis.
Unlike osteoarthritis, which is caused by joint wear and tear, Rheumatoid Arthritis is an autoimmune disorder. It’s a systemic disease that can impact other parts of your body, not just your joints.
Rheumatoid Arthritis has existed for centuries. Evidence of Rheumatoid Arthritis has been found in Native American skeletal remains, suggesting the disease existed long before modern medicine could diagnose or treat it.
Only older people get Rheumatoid Arthritis.
Rheumatoid Arthritis affects people of all ages, including children, though it’s more common in adults between 30 and 60.
Rheumatoid Arthritis affects more than just the joints. Because Rheumatoid Arthritis is an autoimmune disease, it can also impact the heart, lungs, and eyes.
Myth
Rheumatoid Arthritis is just like “normal” arthritis.
Fact
Unlike osteoarthritis, which is caused by joint wear and tear, Rheumatoid Arthritis is an autoimmune disorder. It’s a systemic disease that can impact other parts of your body, not just your joints.
Trivia
Rheumatoid Arthritis has existed for centuries. Evidence of Rheumatoid Arthritis has been found in Native American skeletal remains, suggesting the disease existed long before modern medicine could diagnose or treat it.
Myth
Only older people get Rheumatoid Arthritis.
Fact
Rheumatoid Arthritis affects people of all ages, including children, though it’s more common in adults between 30 and 60.
Trivia
Rheumatoid Arthritis affects more than just the joints. Because Rheumatoid Arthritis is an autoimmune disease, it can also impact the heart, lungs, and eyes.
Effective Treatments for Rheumatoid Arthritis
While there’s currently no cure for rheumatoid arthritis, treatments have advanced significantly, helping people manage symptoms and maintain a good quality of life. Treatment plans typically include a combination of medications, physical therapy, lifestyle changes, and, in some cases, surgery.
1. Medications
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs, like ibuprofen and naproxen, can reduce pain and inflammation.
- Disease-Modifying Antirheumatic Drugs (DMARDs): DMARDs help slow the progression of RA and prevent joint damage.
- Biologic Agents: These target specific parts of the immune system to reduce inflammation, often used when DMARDs aren’t enough.
2. Physical and Occupational Therapy
- Physical Therapy: Exercises can improve your range of motion and keep joints flexible.
- Occupational Therapy: An occupational therapist can teach you methods to perform daily tasks with less pain.
- Alternative Therapies: Some people find relief with acupuncture, yoga, and supplements, though you should discuss these with your doctor before starting.
3. Lifestyle Changes
- Exercise: Low-impact exercises like swimming or walking can strengthen muscles and protect joints.
- Diet: Anti-inflammatory diets, including foods rich in omega-3 fatty acids and antioxidants, may help manage symptoms.
- Rest and Stress Management: Managing stress and getting adequate rest are crucial, as RA symptoms can worsen with stress.
4. Surgery
- Joint Replacement: In severe cases, surgery may be recommended to replace damaged joints, often in the hips or knees.
Is Rheumatoid Arthritis Curable?
Currently, there is no cure for Rheumatoid Arthritis. However, many treatments can effectively manage symptoms, reduce inflammation, and help prevent joint damage. Research is ongoing, and treatments have advanced significantly in recent years, providing hope for even better management options in the future.
How Can Caregivers Support Someone with Rheumatoid Arthritis?
If you’re caring for someone with rheumatoid arthritis, there are many ways you can help:
Assist with Daily Tasks: Rheumatoid arthritis pain and fatigue can make routine tasks challenging. Offering help with household chores, cooking, or running errands can make a big difference.
Encourage Physical Activity: Regular, gentle exercise can help manage rheumatoid arthritis symptoms. Going for a walk or joining them in low-impact activities can be both supportive and encouraging.
Be Patient and Understanding: Rheumatoid arthritis pain is unpredictable, and your loved one may have “good” and “bad” days. Patience and empathy go a long way in providing emotional support.
Help Manage Flares: During flare-ups, rheumatoid arthritis symptoms can worsen significantly. Having a plan to help manage severe pain, such as knowing when to apply heat or cold, ensuring medications are taken on time, and contacting healthcare professionals when needed, is essential.
Living with rheumatoid arthritis can be challenging, but with a supportive network, the right treatments, and lifestyle adjustments, managing the disease is possible. Although rheumatoid arthritis is not curable, many people with Rheumatoid Arthritis (RA) live fulfilling, active lives. If you or someone you know has RA, educating yourself and working with a healthcare team is a proactive approach that can make a real difference.